Abstract and Introduction
Abstract
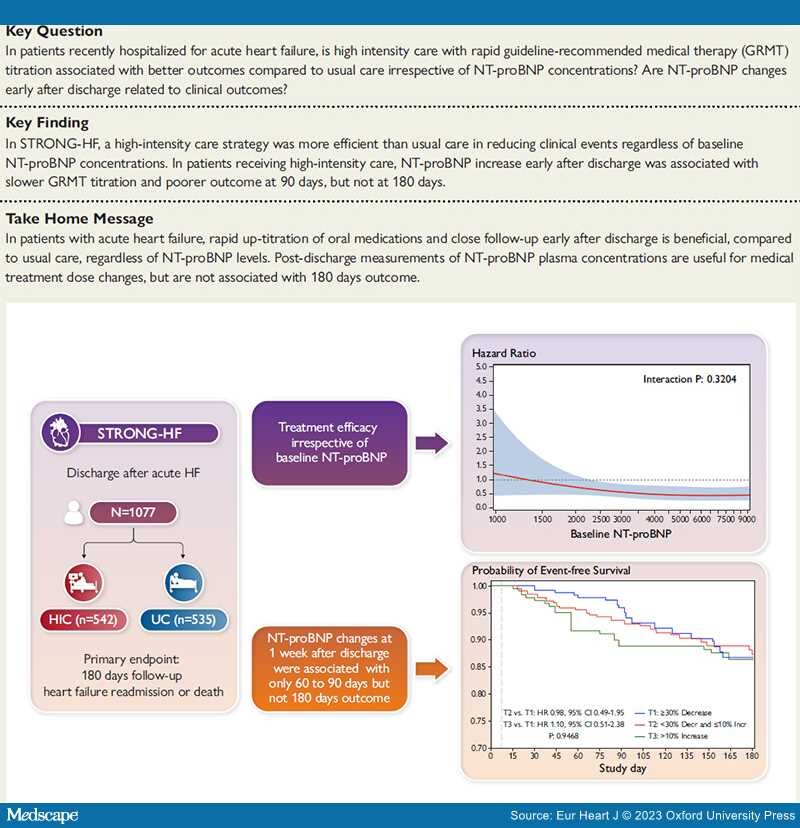
Aims: STRONG-HF showed that rapid up-titration of guideline-recommended medical therapy (GRMT), in a high intensity care (HIC) strategy, was associated with better outcomes compared with usual care. The aim of this study was to assess the role of N-terminal pro-B-type natriuretic peptide (NT-proBNP) at baseline and its changes early during up-titration.
Methods and Results: A total of 1077 patients hospitalized for acute heart failure (HF) and with a >10% NT-proBNP decrease from screening (i.e. admission) to randomization (i.e. pre-discharge), were included. Patients in HIC were stratified by further NT-proBNP changes, from randomization to 1 week later, as decreased (≥30%), stable (<30% decrease to ≤10% increase), or increased (>10%). The primary endpoint was 180-day HF readmission or death. The effect of HIC vs. usual care was independent of baseline NT-proBNP. Patients in the HIC group with stable or increased NT-proBNP were older, with more severe acute HF and worse renal and liver function. Per protocol, patients with increased NT-proBNP received more diuretics and were up-titrated more slowly during the first weeks after discharge. However, by 6 months, they reached 70.4% optimal GRMT doses, compared with 80.3% for those with NT-proBNP decrease. As a result, the primary endpoint at 60 and 90 days occurred in 8.3% and 11.1% of patients with increased NT-proBNP vs. 2.2% and 4.0% in those with decreased NT-proBNP (P = 0.039 and P = 0.045, respectively). However, no difference in outcome was found at 180 days (13.5% vs. 13.2%; P = 0.93).
Conclusion: Among patients with acute HF enrolled in STRONG-HF, HIC reduced 180-day HF readmission or death regardless of baseline NT-proBNP. GRMT up-titration early post-discharge, utilizing increased NT-proBNP as guidance to increase diuretic therapy and reduce the GRMT up-titration rate, resulted in the same 180-day outcomes regardless of early post-discharge NT-proBNP change.
Structured Graphical Abstract
The role of NT-proBNP in patients receiving high intensity care (HIC) after hospital admission for acute heart failure. This analysis from the STRONG-HF trial includes 1077 patients. The treatment effect of a HIC strategy vs. usual care (UC) reduced the primary endpoint regardless of baseline NT-proBNP concentrations. In the 542 patients included in the HIC group, an increase in NT-proBNP levels was associated with a poorer outcome up to 90-day follow-up, but not at 180 days. CI, confidence interval; HF, heart failure; HR, hazard ratio; NT-proBNP, N-terminal pro-B-type natriuretic peptide.
Introduction
N-terminal pro-B-type natriuretic peptide (NT-proBNP) has a major role in the diagnosis and risk stratification of patients with heart failure (HF).[1–3] However, its role in the titration of guideline-recommended medical therapy (GRMT) remains unsettled. The Safety, Tolerability and Efficacy of Rapid Optimization, Helped by NT-proBNP Testing, of Heart Failure Therapies (STRONG-HF) study[4–6] showed the efficacy and safety of a high intensity care (HIC) regimen vs. usual care (UC) in patients recently hospitalized for acute HF. N-terminal pro-B-type natriuretic peptide measurements had a major role in this trial. First, they were used as enrolment criteria as patients had to have NT-proBNP concentrations at screening >2500 pg/mL with >10% decrease between screening and randomization with values >1500 pg/mL at randomization. Second, NT-proBNP measurements were repeated at 1-, 2-, 3-, and 6-week follow-up visits in the HIC regimen group and physicians were recommended not to up-titrate beta-blocker and to increase diuretic dose when NT-proBNP concentrations were >10% higher than at pre-discharge. In the pre-specified subgroup analysis of STRONG-HF, there was a trend towards a larger benefit of HIC vs. UC in patients with NT-proBNP levels above median, but without significant interaction.[4]
Our present analysis tested two main hypotheses. First, the safety and efficacy of HIC vs. UC may have been different across patients with different NT-proBNP values at baseline. Second, we hypothesized that a HIC strategy of diuretic dose escalation and slower titration of GRMT in response to NT-proBNP increase might have mitigated, if not neutralized, the prognostic impact of early NT-proBNP changes on long-term outcome. Thus, the aim of this study was to examine the relation between baseline NT-proBNP levels and the efficacy of HIC vs. UC, as well as the prognostic significance of changes in NT-proBNP concentrations during follow-up in the HIC group.
Eur Heart J. 2023;44(31):2947-2962. © 2023 Oxford University Press
Copyright 2007 European Society of Cardiology. Published by Oxford University Press. All rights reserved.